Human Health
Residents of the Midwest are already experiencing adverse health impacts from climate change, and these impacts are expected to worsen in the future. The risks are especially high for people whose age, income level, or amount of social connectivity make them more vulnerable.
Air quality
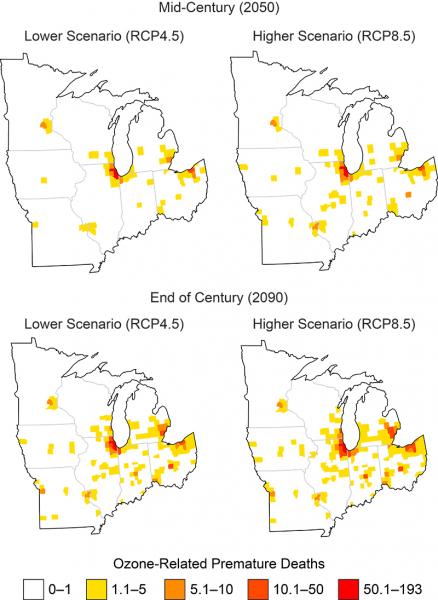
A changing climate is associated with an increase the frequency of meteorological conditions that lead to poor air quality. Increases in ground-level ozone and particulate matter are associated with the prevalence of various lung and cardiovascular diseases, which can lead to missed school days, hospitalization, and premature death.
In the absence of mitigation, ground-level ozone concentrations are projected to increase across most of the Midwest, resulting in an additional 200 to 550 premature deaths in the region per year by 2050. These effects could cost an estimated $4.7 billion (in 2015 dollars).
Pollen production has been on the rise in the Midwest, with pollen seasons starting earlier and lasting longer. People with asthma and other respiratory diseases are especially vulnerable to aeroallergens, which can cause allergic rhinitis and exacerbate asthma and sinusitis. Oak pollen alone could be responsible for an annual increase of 88 to 350 asthma-related emergency room visits by 2050, with an estimated average annual cost ranging between $43,000 and $170,000 (in 2015 dollars).
Temperature
Increased daytime and nighttime temperatures in the Midwest are associated with heat-related diseases and death. Extreme heat in urban centers can cause dangerous working and living conditions; high rates of heat-related illness are also present in rural populations, where occupational exposure to heat and access to care is a concern. Exposure to high temperatures has negative impacts on workers’ health, safety, and productivity.
Future risk of heat-related disease could be significantly higher. Climate projections indicate that the Midwest may have the largest increase in extreme temperature-related premature deaths, compared to other U.S. regions where worsening heat is expected to occur. Communities in the northern Midwest and vulnerable populations that typically have not experienced high temperatures may be at risk for heat-related disease and even death.
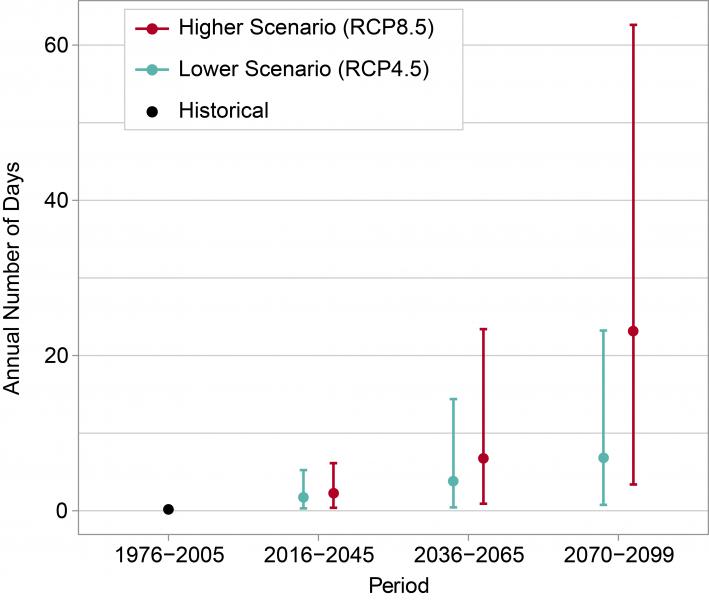
Currently, days over 100°F in Chicago are rare, but they may become more common under both the lower and higher emission scenarios used to produce climate projections. Near the upper end of the model results at late-century—with the potential for almost 60 days per year over 100°F—conditions in Chicago could be more typical of present-day Las Vegas.
Rising temperatures will translate into economic costs among the workforce and in utility bills, potentially exacerbating existing health disparities among those most at risk. By 2050, increased temperatures under the higher emissions scenario are estimated to cost around $10 billion (in 2015 dollars) due to premature deaths and lost work hours; increased electricity demand is estimated to amount to $1.2 billion by 2090 (in 2015 dollars). For those who are chronically ill or reliant on electronic medical devices, the increased cost of electricity may introduce financial and health burdens.
Precipitation
An increase in extreme precipitation and storm events can lead to increased flooding. Riverine flooding can flood streets and low-lying areas, resulting in drinking water contamination, evacuations, damage to buildings, injury, and death. Flooded buildings can experience mold growth that can trigger asthma attacks and allergies during clean-up efforts. Mental stress following flooding events can cause substantial health impacts, including sleeplessness, anxiety, depression, and post-traumatic stress disorder. Precipitation events can carry pathogens that cause gastrointestinal illnesses, putting populations who rely on untreated groundwater—such as wells, which many midwestern communities use as their drinking water sources—at an increased risk of disease.
Unlike flooding, drought is a slow-moving stressor—but it too can cause stress, anxiety, and depression. Drought can cause businesses that rely on water, such as farms and landscape companies, to suffer economic losses and can result in job loss for people who work in these areas. Drought can also change the amount and patterns of certain diseases, such as West Nile virus and Valley Fever, and can worsen asthma and other heart and lung diseases by intensifying wildfires and dust storms, resulting in a higher number of particulates in the air. Drought can intensify heatwaves, causing an increased risk of injury and death from heat exhaustion or heat stroke, and can stress city- or county-wide water systems that supply water not only to households, but also to at-risk populations such as people in hospitals and nursing homes.1
Habitat conditions
Climate-related changes in habitats for disease-carrying insects are associated with higher rates of infection—including the mosquito (Culex pipiens and Culex tarsalis) that transmits West Nile Virus and the blacklegged or deer tick (Ixodes scapularis) that transmits Lyme disease. Northern expansion of the Culex species in the Midwest is expected to result in upwards of 450 additional West Nile Virus cases per year above the 1995 baseline by 2090, absent greenhouse gas mitigation.
Harmful algal blooms can introduce cyanobacteria into drinking and recreational water sources, resulting in restrictions on access and use. Contact with and consumption of water contaminated with cyanobacteria is associated with skin and eye irritation, respiratory illness, gastrointestinal illness, and liver and kidney damage. The occurrence of higher water temperatures, increased runoff, and nutrient-rich habitats—all conditions that encourage cyanobacteria growth—are projected to increase in the Midwest.
Adaptation
Coordination across public health, emergency management, planning, and communication agencies can maximize outreach about the health impacts of climate change to the most at-risk populations and direct coordinated activities to reduce health disparities and impacts.
Public health agencies in the Midwest have developed interdisciplinary communities of practice around climate and health adaptation efforts, enhancing the resilience of the region’s public health systems. Increased surveillance of climate-sensitive exposures and disease are gaining momentum and interest among practitioners and researchers.
Climate mitigation actions can result in co-benefits for health and other outcomes, such as economic development. For example, reducing emissions from energy production and transportation may involve changes to fuel sources, vehicle technology, land use, and infrastructure, while active transportation, such as biking and walking, has been found to significantly decrease disease burden.
Opportunities abound in the Midwest to prioritize active living to reduce climate change drivers and improve health.
Except where footnoted, the preceding text is excerpted and abridged from the report Impacts, Risks, and Adaptation in the United States: Fourth National Climate Assessment, Volume II (Chapter 21, Midwest).
To learn more about climate impacts on human health, visit the Health topic.
- 1National Center for Environmental Health, Division of Environmental Hazards and Health Effects, 2016: Fact Sheet, Drought and Public Health in the U.S., Publication CS263437. Atlanta, GA: Centers for Disease Control and Prevention.